In the fast-evolving healthcare landscape, Revenue Cycle Management (RCM) has become a cornerstone for sustaining the financial health of medical practices, hospitals, and healthcare organizations. With rising administrative complexities, payer rules, and compliance standards, healthcare providers are turning to Healthcare Revenue Cycle Management Services to ensure seamless financial performance and operational efficiency.
This guide explores the importance, process, benefits, and impact of RCM services in modern healthcare.
What Is Revenue Cycle Management (RCM)?
Revenue Cycle Management (RCM) refers to the financial process that healthcare organizations use to track patient care episodes from registration and appointment scheduling to the final payment of a balance. It integrates clinical, administrative, and financial data to ensure that healthcare providers get paid for the services rendered.
In simple terms, RCM is the backbone of healthcare finance — managing every stage of the payment lifecycle, including claims processing, payment posting, denial management, and patient billing.
The goal is to reduce claim denials, minimize revenue leakage, and improve overall cash flow.
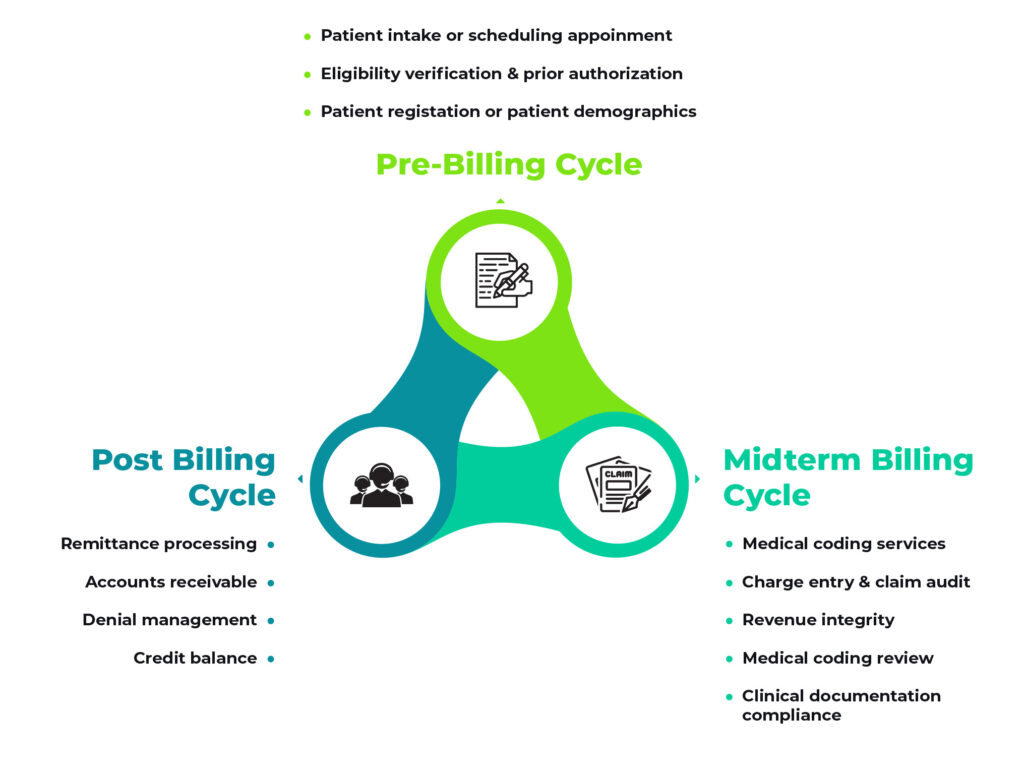
Key Components of Revenue Cycle Management
Effective RCM involves a series of interconnected steps. Let’s break down the major components:
1. Patient Registration and Verification
The RCM process begins with accurate patient registration. This includes collecting patient demographics, insurance details, and verifying eligibility and benefits. Any errors at this stage can cause claim denials or payment delays.
2. Charge Capture
Once medical services are provided, the details must be accurately captured and translated into billable codes using CPT (Current Procedural Terminology) and ICD-10 coding systems. Correct coding ensures compliance and proper reimbursement.
3. Claim Submission
After charge capture, claims are submitted electronically to insurance companies. Clean claim submissions help reduce rejections and speed up reimbursements.
4. Payment Posting
When payments are received from payers, they must be posted accurately into the billing system. This process ensures that financial records are up to date and discrepancies can be quickly identified.
5. Denial Management
Denials are a common issue in healthcare billing. Effective RCM services analyze denial reasons, correct errors, and resubmit claims promptly to recover lost revenue.
6. Patient Collections
After insurance payments, patients may still owe copays or deductibles. Clear communication and patient-friendly billing systems improve collection rates and patient satisfaction.
7. Reporting and Analytics
Comprehensive reporting helps healthcare organizations monitor financial performance, identify bottlenecks, and make data-driven decisions for revenue optimization.
Why Revenue Cycle Management Services Are Essential
Running an in-house RCM department requires expertise, technology, and ongoing compliance monitoring. That’s why many healthcare organizations outsource their RCM services to specialized companies that handle end-to-end billing and collections.
Here are the key reasons why outsourcing RCM is beneficial:
1. Enhanced Cash Flow
RCM providers streamline the billing and collection process, ensuring faster reimbursements and reduced accounts receivable (A/R) days. This leads to steady cash flow and financial stability.
2. Reduced Administrative Burden
Managing billing internally can drain time and resources. Outsourcing allows healthcare staff to focus on patient care while experts manage financial workflows efficiently.
3. Fewer Claim Denials
With advanced analytics, automated claim scrubbing, and compliance checks, RCM companies drastically reduce claim rejections and denials.
4. Compliance with Regulations
Healthcare billing must comply with complex standards such as HIPAA, CMS guidelines, and payer-specific rules. RCM providers ensure adherence to these regulations, protecting your organization from costly penalties.
5. Cost Efficiency
Hiring, training, and retaining in-house billing staff can be expensive. Outsourced RCM solutions offer scalable services at lower operational costs.
6. Data Transparency and Reporting
Modern RCM systems provide detailed insights into claim statuses, payment trends, denial patterns, and revenue forecasts — helping organizations make smarter business decisions.
How RCM Services Improve Healthcare Practice Efficiency
Revenue Cycle Management goes beyond billing; it plays a vital role in enhancing operational performance and patient satisfaction.
-
Improved Workflow Efficiency: Automating tasks like eligibility checks and claim submission saves time and reduces human errors.
-
Better Patient Experience: Transparent billing and quick resolution of financial queries enhance patient trust.
-
Predictable Revenue Streams: With fewer denials and faster collections, providers can forecast revenue accurately.
-
Scalable Growth: RCM systems grow with your practice, supporting expansion and higher patient volumes without financial disruption.
Technology in Modern RCM Services
The digital transformation of healthcare has redefined how RCM services operate. Leading providers leverage AI, automation, and analytics to maximize revenue and minimize errors.
1. Artificial Intelligence (AI) and Machine Learning
AI-based systems predict denials, flag missing data, and recommend corrections before claim submission — preventing revenue loss proactively.
2. Robotic Process Automation (RPA)
RPA automates repetitive tasks such as claim entry, status checks, and payment posting, freeing up staff for higher-value activities.
3. Cloud-Based Platforms
Cloud RCM software ensures secure access to billing data anytime, anywhere. It also improves collaboration between providers and billing teams.
4. Data Analytics and Reporting Tools
Advanced dashboards provide real-time insights into KPIs such as claim turnaround time, denial rates, and revenue recovery metrics.
Industries That Benefit from RCM Services
Revenue Cycle Management is vital across various healthcare segments, including:
-
Hospitals and Health Systems
-
Private Practices and Clinics
-
Behavioral Health and ABA Therapy Providers
-
Urgent Care and Ambulatory Services
-
Dental and Chiropractic Clinics
-
DME (Durable Medical Equipment) Providers
Regardless of the size or specialty, every healthcare organization can benefit from professional RCM support to maintain a strong financial foundation.
Choosing the Right Revenue Cycle Management Partner
When selecting an RCM service provider, consider the following key factors:
-
Experience and Expertise – Choose a company with deep industry knowledge and proven results across healthcare specialties.
-
Technology Stack – Ensure they use secure, modern RCM platforms with AI-driven analytics.
-
Transparency – Look for clear communication, regular performance reports, and full visibility into financial operations.
-
Compliance and Security – The provider should be HIPAA-compliant and adhere to strict data security protocols.
-
Scalability – Select a partner that can grow with your organization and adapt to future needs.
A good RCM partner not only manages billing but also acts as a strategic advisor, helping you identify trends and improve financial outcomes.
Future of Revenue Cycle Management
The future of RCM is data-driven, patient-centered, and automation-powered. As value-based care and digital health continue to evolve, RCM solutions will focus more on predictive analytics, interoperability, and patient engagement.
Healthcare providers will increasingly rely on integrated RCM systems that connect financial and clinical data seamlessly — reducing inefficiencies and ensuring long-term sustainability.
Conclusion
Revenue Cycle Management Services are essential for any healthcare organization aiming to maintain financial health, compliance, and operational excellence. From patient registration to final payment, every step of the RCM process impacts cash flow and patient satisfaction.
Outsourcing to an experienced RCM service provider helps healthcare practices reduce denials, accelerate payments, and focus on what truly matters — delivering quality patient care.
By embracing automation, data analytics, and expert-driven processes, your organization can achieve consistent revenue growth and long-term success in today’s competitive healthcare environment.