Revolutionizing Healthcare Administration Through Professional Third-Party Services
The healthcare industry continues to transform rapidly, with technological advancements and regulatory changes reshaping how medical insurance operates across global markets. Third-party administrators have emerged as essential facilitators in this complex ecosystem, managing the intricate relationships between healthcare providers, insurance carriers, and policyholders. These specialized organizations handle everything from policy administration to claims adjudication, ensuring smooth operations while maintaining cost efficiency. In regions experiencing rapid economic growth and population expansion, the demand for professional healthcare administration has never been higher. The ability to process thousands of claims daily while maintaining accuracy and compliance requires sophisticated systems, experienced personnel, and unwavering commitment to service excellence that defines successful operations in this competitive landscape.
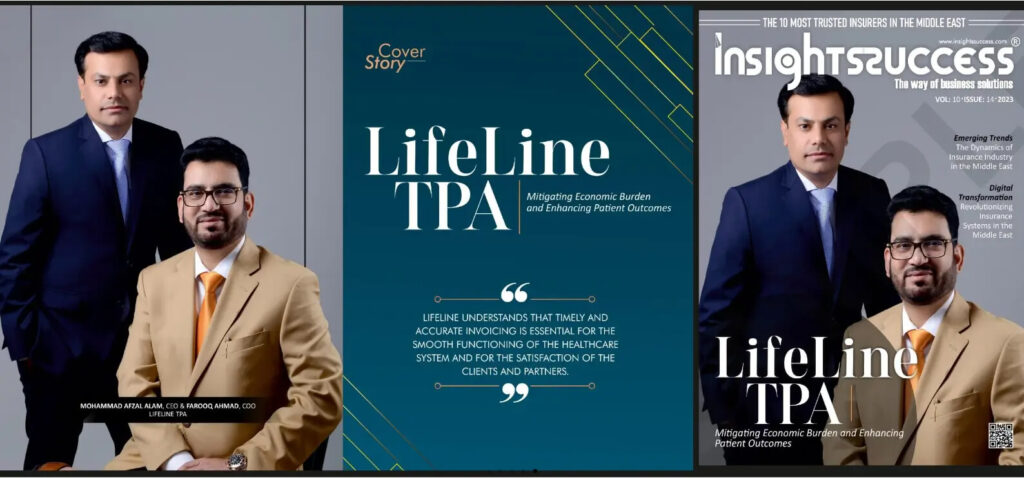
Expert Management Solutions from Life Line TPA
Navigating the healthcare insurance sector requires partnering with experienced administrators who understand regional nuances and international standards. life line tpa has established itself as a premier healthcare management company since its inception in 2015, delivering exceptional services across the UAE, Oman, and Turkey. The organization specializes in comprehensive claims administration, including processing, settlement, reconciliation, and meticulous record-keeping that ensures regulatory compliance. Their innovative approach combines cutting-edge technology with human expertise, utilizing advanced adjudication rules that automatically process the majority of claims without requiring manual review. This automation significantly reduces processing times while minimizing errors, creating a seamless experience for both insurance companies and their members. The organization maintains strategic partnerships with insurance carriers and reinsurance companies, facilitating effective risk distribution and financial stability across the healthcare ecosystem.
Simplified Documentation Process Using the Lifeline Claim Form
Submitting insurance claims should never add stress to already challenging medical situations, which is why streamlined documentation processes are essential for patient satisfaction. The lifeline claim form represents a carefully designed solution that balances thoroughness with simplicity, capturing all required information without overwhelming users with unnecessary complexity. This standardized documentation approach reduces common errors that typically cause claim delays or denials, helping members receive reimbursements faster. Accessibility stands as a key priority, with forms available through digital platforms including web portals and mobile applications, allowing submissions from any location with internet connectivity. The digital infrastructure supports document uploads, enabling members to attach medical reports, prescriptions, and invoices directly to their claims. Real-time tracking features keep policyholders informed throughout the adjudication process, providing transparency that builds confidence in the system. Emergency situations receive priority handling, with dedicated pathways ensuring that urgent claims receive immediate attention from specialized teams trained to make rapid decisions without compromising accuracy.
Comprehensive Network Solutions in TPA Insurance
Effective healthcare administration extends far beyond claims processing to encompass robust network management that connects members with quality medical providers. The scope of tpa insurance services includes establishing and maintaining relationships with hospitals, clinics, diagnostic centers, and pharmacies throughout service regions. These carefully curated networks provide cashless access to insured members, eliminating the financial barriers that often delay necessary medical treatment. Provider credentialing processes evaluate facilities and practitioners based on rigorous criteria including qualifications, equipment standards, patient safety records, and clinical outcomes. Ongoing monitoring ensures continued compliance with established quality benchmarks while negotiating favorable fee arrangements that control costs without compromising care quality. The extensive network spans the entire GCC region, offering members choice and convenience regardless of their location. Specialized networks address specific needs, from routine primary care to complex tertiary treatments requiring advanced medical expertise. This comprehensive approach ensures that every member can access appropriate care when needed, with the administrative support necessary to facilitate smooth, cashless transactions at point of service.
Professional Growth Through Lifeline Career Development
The healthcare administration field offers rewarding opportunities for individuals seeking meaningful careers that positively impact communities. A lifeline career path provides the chance to work in a dynamic environment where medical knowledge, analytical thinking, and customer service skills converge to solve real-world challenges. The organization employs diverse professionals including medical directors, claims analysts, customer service specialists, network coordinators, and technology experts who collaborate to deliver exceptional results. Investment in human capital remains a cornerstone of operational philosophy, with comprehensive training programs ensuring that team members develop the expertise needed to excel in their roles. New employees participate in extensive onboarding that covers industry regulations, medical terminology, insurance principles, and company-specific systems and procedures. Continuing education opportunities keep staff current with evolving healthcare practices, coding updates, and technological innovations. Career advancement pathways recognize and reward excellence, with internal promotion opportunities available for those demonstrating exceptional performance and leadership potential. The work environment emphasizes collaboration, innovation, and continuous improvement, fostering a culture where employees feel valued and motivated to contribute their best efforts daily.
Innovation Through Technology and Member Experience
Digital transformation has fundamentally changed healthcare administration, enabling capabilities that were impossible just years ago. Sophisticated platforms now integrate artificial intelligence algorithms that detect patterns in claims data, identifying potential fraud while streamlining legitimate transactions. Predictive analytics help forecast healthcare utilization trends, allowing proactive resource allocation and cost management strategies. Member-facing technologies have evolved beyond basic information portals to become comprehensive health management tools. The mobile application provides instant access to digital membership cards, provider directories with real-time availability, wellness program resources, and personalized health recommendations. Push notifications keep members informed about claim status updates, upcoming renewals, and important policy information. The round-the-clock call center operates continuously, staffed by multilingual representatives trained to handle diverse inquiries ranging from coverage questions to emergency authorization requests. This omnichannel approach ensures that members can connect through their preferred communication method, whether phone, email, chat, or social media. User experience design principles guide all digital developments, prioritizing intuitive navigation and clear information presentation that empowers members to manage their healthcare confidently.
Building Sustainable Partnerships Across the Healthcare Ecosystem
Long-term success in healthcare administration depends on cultivating strong, mutually beneficial relationships with numerous stakeholders. The organization collaborates with leading insurance providers including major carriers that trust its expertise to manage their health insurance portfolios effectively. These partnerships are founded on shared values of transparency, accountability, and member-centered service delivery. Regular communication channels facilitate quick resolution of issues while strategic planning sessions align future initiatives with market opportunities. Healthcare provider relationships receive equal attention, with dedicated account managers ensuring that network facilities receive timely payments, clear communication about policy changes, and support in navigating administrative requirements. This balanced approach recognizes that excellent service requires cooperation from all participants in the healthcare delivery chain. Industry engagement extends to participating in regulatory discussions, contributing to standards development, and collaborating with professional associations to advance best practices. The commitment to ethical business conduct and transparent operations has earned recognition from peers and regulators alike, establishing a reputation for integrity that attracts quality partners.
Ensuring Quality Through Rigorous Standards and Oversight
Healthcare administration carries significant responsibility for decisions that directly affect patient wellbeing and financial security, demanding uncompromising attention to quality and compliance. Comprehensive internal controls monitor every operational aspect, from initial data entry through final claim payment, with multiple verification checkpoints preventing errors and detecting irregularities. Fraud prevention systems employ advanced analytics to identify suspicious patterns, protecting the integrity of insurance pools while ensuring that legitimate members receive entitled benefits. Regular audits by independent assessors verify compliance with regulatory requirements and internal policies, providing objective evaluation of performance. Quality metrics track processing accuracy, turnaround times, customer satisfaction scores, and financial performance, enabling data-driven management decisions. Continuous improvement initiatives systematically identify opportunities to enhance efficiency, reduce costs, and improve service quality. The vision extends beyond regional operations to aspire toward global excellence in healthcare administration. This ambitious outlook drives constant innovation and refinement of processes, systems, and service delivery models that set new industry standards for performance and reliability.