Billing for mental health services plays a vital role in maintaining financial stability for behavioral health practices across the United States. Unlike general medical billing, mental health billing follows unique payer rules, authorization requirements, and documentation standards. Even small errors can result in denied claims, delayed reimbursements, or compliance risks. Understanding the fundamentals of mental health billing helps providers improve cash flow, reduce administrative stress, and focus more on delivering quality patient care. This blog explains how mental health billing works, common challenges, best practices, and answers to frequently asked questions.
Mental health billing refers to submitting insurance claims for services provided by licensed professionals such as psychiatrists, psychologists, licensed clinical social workers, counselors, and therapists. These services include psychiatric evaluations, psychotherapy sessions, medication management, crisis intervention, and tele mental health visits. Mental health billing is also called behavioral health billing and often differs from traditional medical billing, making specialized billing knowledge extremely important.
Commonly billed mental health services include diagnostic assessments, individual psychotherapy, family therapy, group therapy, and medication management visits. Each service must be reported using the correct Current Procedural Terminology code and supported by clear, accurate documentation. Psychotherapy services are time based, so the selected CPT code must match the actual duration of the session provided to the patient.
Frequently used CPT codes in mental health billing include 90791 for psychiatric diagnostic evaluations without medical services and 90792 for evaluations with medical services. Psychotherapy codes include 90832 for thirty minute sessions, 90834 for forty five minute sessions, and 90837 for sixty minute sessions. Group psychotherapy is commonly billed using 90853. Incorrect CPT code selection remains one of the top reasons for mental health claim denials.
In addition to procedure codes, claims must include valid ICD ten diagnosis codes to establish medical necessity. Common diagnoses include major depressive disorder, generalized anxiety disorder, post traumatic stress disorder, and attention deficit hyperactivity disorder. Diagnosis codes must always align with the provider assessment, treatment plan, and progress notes to meet payer requirements.
Insurance verification and prior authorization are essential before delivering mental health services. Practices should confirm behavioral health benefits, visit limits, patient financial responsibility, and authorization requirements before scheduling appointments. Missing or expired authorizations frequently lead to denied claims and lost revenue.
Accurate documentation is the foundation of successful mental health billing. Providers must maintain complete intake forms, initial evaluations, individualized treatment plans, and detailed progress notes for every encounter. Documentation should clearly demonstrate medical necessity, patient progress, and time spent during therapy while remaining compliant with HIPAA and payer guidelines.
Telehealth has become an important part of mental health care delivery. Most United States payers allow tele mental health billing when appropriate CPT codes, telehealth modifiers, and correct place of service codes are used. Because telehealth rules vary by payer, staying updated is critical.
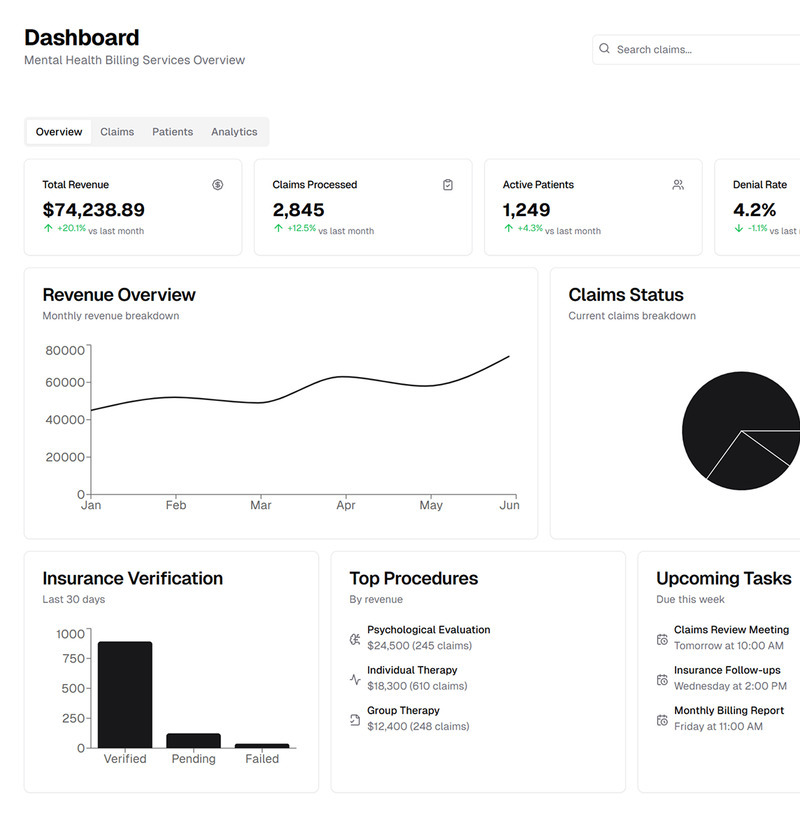
Common mental health billing challenges include coding errors, authorization issues, limited payer coverage, timely filing denials, and documentation gaps. Best practices include verifying eligibility before every visit, submitting clean claims promptly, monitoring denials, and appealing underpaid claims. Many providers outsource mental health billing to experienced revenue cycle management companies to improve accuracy and compliance.
Frequently Asked Questions
What are the most common CPT codes in mental health billing? The most common psychotherapy codes are 90832, 90834, and 90837.
Do mental health services require prior authorization? Many insurance plans require authorization, especially for ongoing therapy services.
Can mental health services be billed through telehealth? Yes, most payers allow tele mental health billing when guidelines are followed.
Who is eligible to bill for mental health services? Licensed and credentialed mental health professionals may bill, depending on payer rules.
Why are mental health claims denied? Common reasons include incorrect coding, missing authorization, and insufficient documentation.
Is outsourcing mental health billing beneficial? Outsourcing often improves reimbursements, reduces denials, and ensures long term compliance for growing practices.