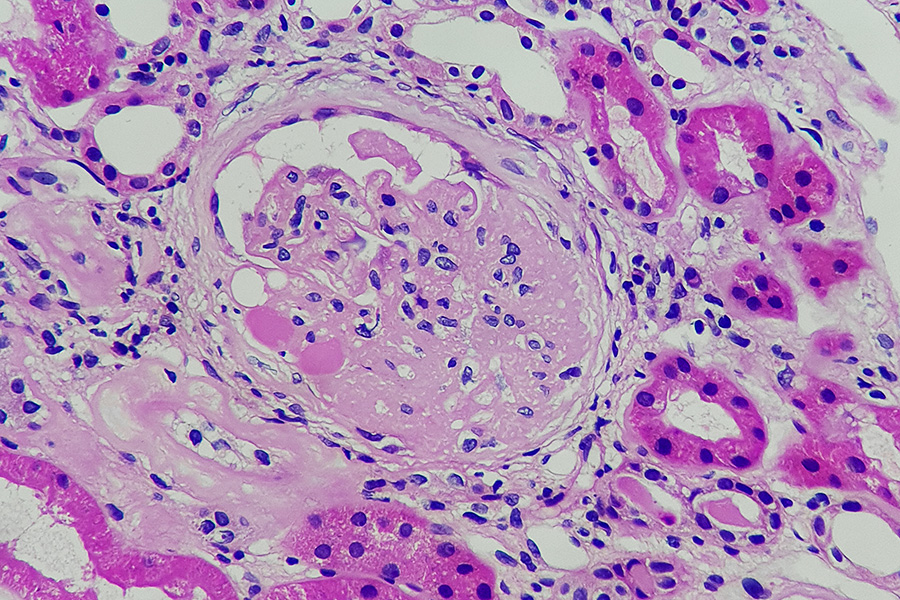
A diagnosis of Focal Segmental Glomerulosclerosis (FSGS) is a serious one. This condition, characterized by scarring in the kidney’s filters (glomeruli), is a leading cause of nephrotic syndrome and often leads to End-Stage Renal Disease (ESRD). Because FSGS is not a single disease but a pattern of injury, managing it effectively means digging deep to find the root cause.
At Neph Cure Inc., we are dedicated to providing clarity in the face of complex kidney conditions. We know that tackling FSGS kidney disease treatment requires a multi-pronged approach: identifying the FSGS risk factors and the underlying FSGS causes before crafting a personalized therapeutic strategy.
This professional post will explore the diverse origins and risk factors associated with FSGS, outline the various underlying FSGS causes, and detail the multifaceted nature of FSGS kidney disease treatment aimed at preserving kidney function and improving long-term outcomes.
Part 1: The Why Behind the Scar—FSGS Causes and Risk Factors
Understanding the FSGS causes is the first step toward effective treatment. The injury that leads to scarring of the podocytes (the specialized filtering cells) can stem from genetic predisposition, underlying systemic diseases, or an unknown immune factor. This knowledge helps categorize the disease and determine the most appropriate therapy.
The Three Categories of FSGS Causes
-
Primary (Idiopathic) FSGS:
-
The Cause: No identifiable cause, but strongly linked to a hypothesized circulating permeability factor in the blood. This factor directly injures the podocytes.
-
Risk Factors: Often presents with severe nephrotic syndrome (massive protein loss) and is more common in younger adults.
-
Treatment Hint: This form is often treated with immunosuppressive therapy to neutralize the unknown factor.
-
-
Genetic (Familial) FSGS:
-
The Cause: Caused by inherited mutations in genes ($NPHS2$, $WT1$, $APOL1$, etc.) that encode proteins essential for the structure and function of the podocytes.
-
Risk Factors: A family history of kidney disease or kidney failure, onset often in childhood or young adulthood, and resistance to steroid therapy.
-
Treatment Hint: Treatment focuses on supportive care (ACE inhibitors) since the issue is structural, not immune-driven.
-
-
Secondary FSGS:
-
The Cause: The scarring is an adaptive response of the glomeruli to chronic stress, high workload, or injury from a known external source.
-
Risk Factors: This category has the clearest associated risk factors, including:
-
Severe Obesity: The metabolic stress and hyperfiltration required to support high body mass can injure podocytes.
-
Uncontrolled Chronic Hypertension (High Blood Pressure): Damages the kidney blood vessels and increases pressure within the glomeruli.
-
Reduced Nephron Mass: Previous injury, surgery (like nephrectomy), or congenital absence of a kidney forces the remaining filters to overwork (hyperfiltration).
-
Viral Infections: Such as HIV (HIV-Associated Nephropathy, or HIVAN).
-
Drug Toxicity: Certain medications can occasionally induce FSGS.
-
-
APOL1 Kidney Disease: A Critical Genetic Risk
A significant Focal Segmental Glomerulosclerosis risk factor for individuals of African descent is the presence of high-risk variants (G1 and G2) of the APOL1 gene. Having two copies of these high-risk alleles drastically increases the likelihood and accelerates the progression of FSGS and other related kidney diseases. APOL1 status is now a crucial piece of the diagnostic puzzle, guiding prognosis and transplant decisions.
Part 2: The Action Plan—FSGS Kidney Disease Treatment
Because the FSGS causes are so varied, FSGS kidney disease treatment must be highly individualized. A single treatment protocol does not work for everyone. Effective management relies on a combination of specific therapy to target the cause and supportive therapy to protect the remaining kidney function.
Specific Therapy (Targeting the Cause)
-
Immunosuppression: Reserved primarily for Primary FSGS (the presumed immune-mediated form). Medications like corticosteroids (prednisone) and calcineurin inhibitors (cyclosporine or tacrolimus) are used to suppress the damaging immune response and induce remission of proteinuria.
-
Targeting APOL1: For APOL1 kidney disease, specific small-molecule inhibitors designed to block the toxic function of the APOL1 protein are in development and entering clinical trials, representing the future of gene-specific treatment.
-
Addressing Secondary Causes: The single most important step for Secondary FSGS is removing the risk factor. This means aggressive blood pressure control, significant weight loss for obesity-related FSGS, or treating the underlying viral infection.
Supportive Therapy (Protecting the Kidney)
Regardless of the cause, every patient with FSGS requires therapies to slow the progression of scarring:
-
ACE Inhibitors or ARBs: These medications (Angiotensin-Converting Enzyme inhibitors or Angiotensin II Receptor Blockers) are the cornerstone of FSGS kidney disease treatment. They reduce blood pressure and, critically, reduce the pressure within the glomeruli, which significantly lowers the amount of protein leakage (proteinuria) and slows the rate of kidney function decline.
-
Fluid and Edema Control: Diuretics (water pills) are used to manage the severe swelling (edema) caused by nephrotic syndrome. A strict low-sodium diet is essential for these medications to work effectively.
-
Cholesterol Management: Statins are often prescribed to manage the high cholesterol and triglyceride levels (hyperlipidemia) that accompany nephrotic syndrome, which helps reduce the risk of cardiovascular disease.
Part 3: Lifestyle as Medicine—Managing Risk Factors Daily
While genetics and immune factors play a massive role, managing modifiable FSGS risk factors through diet and lifestyle provides the patient with the most control over their disease journey.
Key Lifestyle Interventions
-
Aggressive Blood Pressure Control: High blood pressure is both a cause of FSGS (secondary) and a major accelerator of kidney decline in all types. Aim for blood pressure targets set by your nephrologist (often $< 130/80 text{mmHg}$).
-
Sodium Restriction: A low-sodium diet (under 2,000 mg per day) is crucial for managing hypertension and edema. Reducing salt intake minimizes the need for high doses of diuretics and maximizes the benefit of ACE/ARB therapy.
-
Weight Management: For obesity-related FSGS, achieving and maintaining a healthy weight can lead to a reduction in proteinuria and, in some cases, remission.
-
Dietary Protein: Consult a renal dietitian to determine the appropriate amount of protein intake. Too much can stress the remaining filters, while too little can lead to malnutrition, especially given the protein loss from nephrotic syndrome.
-
Avoid Nephrotoxic Drugs: Avoid frequent or high-dose use of NSAIDs (Non-Steroidal Anti-Inflammatory Drugs like ibuprofen or naproxen), as they can acutely harm kidney function.
Neph Cure Inc.: Our Vision for Personalized FSGS Treatment
The path to an effective FSGS kidney disease treatment is rarely simple. It demands a detective’s mindset to uncover the exact FSGS causes—is it an immune attack that needs suppression, a genetic flaw that needs supportive care, or an external risk factor that needs removal?
At Neph Cure Inc., we champion the use of advanced diagnostics, including genetic screening for APOL1 and other mutations, to classify the disease accurately. This precision medicine approach ensures that your treatment plan is tailored to the specific mechanism of your illness, offering the best chance for long-term kidney survival.
We are committed to accelerating research into new targeted therapies and providing clear, actionable information to help you manage the modifiable FSGS risk factors today.
Ready to partner with experts in navigating the challenges of FSGS?
Contact Neph Cure Inc. today to explore our resources and commitment to precision nephrology.